May is Older Americans Awareness Month:
The Revolution in Longevity Has Created Opportunities and Risks

You may be older than you used to be, but you’re still the person you always were. That’s a message younger people need to learn. A 70-, 75- or 80-year-old person, whether robust and fit, or even if compromised in some way, is often still active and fully involved in living – an individual, not a geriatric leftover.
Getting older doesn’t have to be all aches and pains. In fact, studies have shown that older people are happier than those in the middle period of their lives, even if they have health or other issues.
Years ago, people didn’t realize that they could lengthen their active years, sometimes by decades, by taking steps to maintain their mental and physical health. In recent years, science has shown that diet, exercise, community connection, good sleep habits, and a sense of purpose can improve people’s health and mental faculties, and often dramatically lengthen their lives.
Medicines and medical equipment have also extended lives. Heart disease is being fought on many fronts, as is cancer in all its forms. Joint replacements and diabetes management have involved high tech medical equipment that has been miraculous for millions.
Physical changes do come with the passing of time, but again, people have learned to take preventive measures to limit or postpone the risks and negative effects. Learning about fall prevention, balance and strength exercises, protecting skin against sun damage, and wearing sunglasses to prevent cataracts are all actions people have learned to take, to help them avoid problems and continue to enjoy their lives.

One of the challenges people face when they live far longer than they used to, is that they may need care and assistance in their homes or in a residential facility for a decade or more. They can still live satisfying lives, but they need assistance with some of their activities. With families far more spread out than was the case decades ago, this care is often provided by paid caregivers.
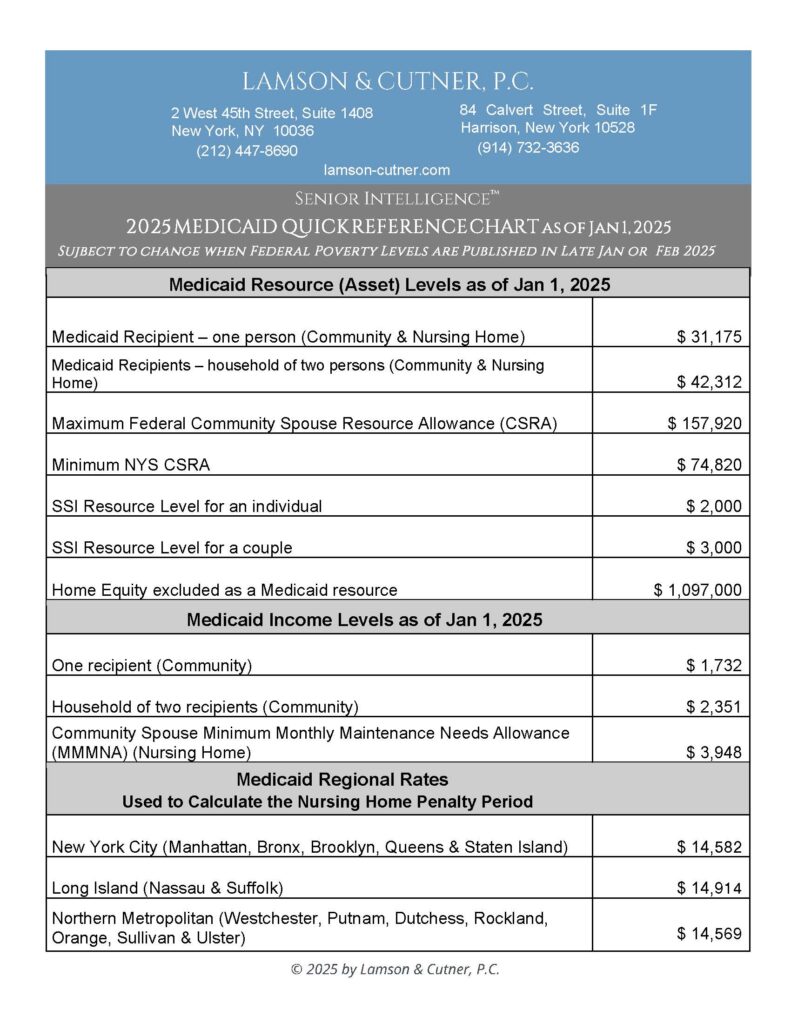
People who begin needing care often don’t realize until well into their assistance-needing period, that caregiving can be a disastrous drain on their finances. Caregivers aren’t getting rich, but they need to be paid, and home health companies have both legwork and paperwork for which they need to be compensated.
The combination of these factors means that costs can skyrocket, and the net result of paying for care is often that people’s entire life savings are wiped out. People try to reduce the cost of care by paying their caregivers in cash. Not only is this illegal, it exposes the employer to enormous liability, should the caregiver be injured on the job.
The attorneys at Lamson & Cutner feel it is crucial for older people, and the children or loved ones of those older people, to be informed. Learning about the financial risks of long-term care costs, and about the opportunities that are available to protect them against these risks, will enable those who need long-term care to maintain their lifestyles to the greatest extent possible.
Our firm spends a lot of time and energy on educating people about issues surrounding long-term care. We have worked to make our website informative, understandable and useful. In addition, we have a very busy speaking schedule. We are authorized to give CEU credits to health care professionals and social workers. We also give general-interest presentations at senior centers, houses of worship, and other venues, to people who might face long-term care costs for themselves or others.
Becoming informed – and taking action – are your best defenses against both the physical and financial risks that come with age. You’re never too old to start. Learn, act, and live your best life!